What are Dendritic Cells?
Meet the Powerhouses Orchestrating Your Body’s Immune Responses
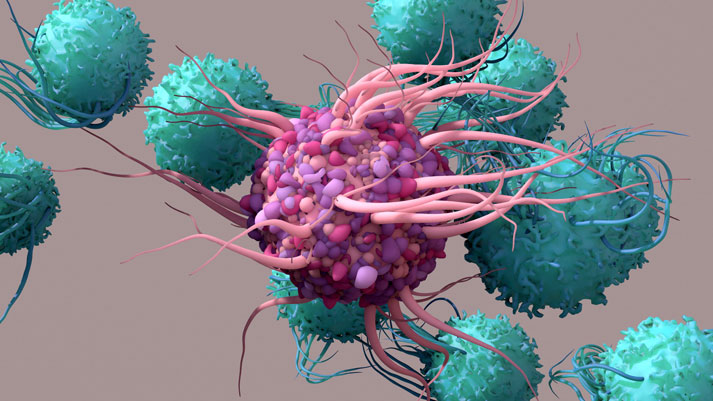
Dendritic cells represent a specialized category of immune cells crucial for coordinating our body's defense mechanisms against harmful pathogens. Their principal duty is to capture and present antigens – substances capable of triggering an immune response – to other immune cells. This crucial function not only boosts but also regulates the immune system, ensuring its effectiveness in combating threats.
Dendritic Cells: Professional Antigen Presenting Cells
Dendritic cells, named for their tree-like branched projections called "dendrites," are primary located in tissues that are in contact with the external environment, such as the skin, mucosal surfaces and inner linings of organs. Their strategic placement enables them to capture and process antigens efficiently. Moreover, their elongated projections maximize the cell's surface area, increasing exposure to antigens.
When dendritic cells encounter antigens, they engulf and ingest them through a vital process called phagocytosis. Once inside the cell, the solid antigen particles are broken down into smaller fragments, which are then presented on the surface of the dendritic cell using specialized molecules called major histocompatibility complex (MHC) molecules. This process is known as antigen presentation.
Considered professional antigen presenting cells (APCs), dendritic cells have the unique ability to present antigens to other immune cells, particularly T cells, which are key players in adaptive immunity. When T cells are presented an antigen from a dendritic cells, they become activated and initiate a strategic immune response tailored to the specific antigen encountered.
Moreover, dendritic cells are integral to immune tolerance, a mechanism vital for distinguishing between self- and non-self-antigens and preventing autoimmune reactions. Dendritic cells aid in educating T cells to recognize and tolerate self-antigens – molecules inherently present in the body – while mounting effective defense responses against external threats1,2
Bridging the Gap Between Innate and Adaptive Immunity
While the majority of immune cells are either a part of the innate or adaptive immune response, dendritic cells play a pivotal role as mediators between these two responses. They serve to link the initial recognition of harmful substances by the innate immune system with the specific, tailored responses mounted by the adaptive immune system.
In particular, plasmacytoid dendritic cells (pDCs), a distinct subset of dendritic cells, are instrumental in bridging the innate and adaptive immune responses, essential for coordinating an effective immune response. 3
Upon encountering external stimuli, pDCs swiftly produce and release abundant amounts of type I interferons, including interferon-alpha (IFN-α). Besides their potent antiviral properties, these interferons also prompt the activation of natural killer (NK) cells, fortifying your body’s first-line of defenses.
Additionally, the production of type I interferons primes and activates immune cells central to adaptive immunity, including T cells and B cells, which then coordinate a strategic defense strategy against specific pathogens.4
The unique ability of pDCs to activate multiple key immune cells involved in both the innate and adaptive immune responses has rightfully earned them the title of "leaders of the immune system."
IMMUSE® Postbiotic Activates pDCs for More Comprehensive Immune Support
Recognizing the critical role of pDCs in safeguarding our health, researchers at Kirin specifically set out to discover a strain of lactic acid bacteria capable of stimulating pDC activity.
After testing hundreds of strains, they identified one particular strain, named Lactococcus lactis strain Plasma (or LC-Plasma), which directly activated pDCs, leading to the production of IFN-α. Remarkably, LC-Plasma is the first strain of bacteria clinically shown to stimulate pDC activity.
Cultured using proprietary fermentation technology, the unique strain was then heat-treated to create a postbiotic product and branded IMMUSE®. Below are a few frequently asked questions about IMMUSE® postbiotic answered by Dr. Danielle Citrolo, Vice President of Scientific and Regulatory Affairs at Kyowa Hakko U.S.A., Inc.
Once orally taken, how long does it takes to see IMMUSE’s effects on pDC activity?
Dr. Citrolo: The shortest research showed a benefit after 4 weeks. That is mostly because we are hoping for a pathogen exposure to show its impact. Although the way it works we do anticipate it would have an immediate effect on the existing pDCs.
Are the pDC effects apparent after a single dose or does it take several days to build?
Dr. Citrolo: We are constantly making new pDCs so it is good to have consistent exposure so the new pDCs are activated by IMMUSE and help prime your immune cells.
How long would the effect on pDCs be sustained after you stop taking it?
Dr. Citrolo: The life cycle of pDCs varies greatly however, if activated it could be as long as two weeks. I think after a week it will start to fade and then most of the effect will be gone by 2 weeks.
Learn more about groundbreaking IMMUSE® postbiotic, an advanced immune health ingredient revolutionizing comprehensive immune support. Explore its distinctive mechanism of action, backed by insights from three clinical trials highlighted below.
Spotlight on Functional Immune Health
1Liu K. Dendritic Cells. Encyclopedia of Cell Biology. 2016:741–9.
2Sidharthan, Chinta. "What are Dendritic Cells?". News-Medical. 31 March 2024.
3Novak N, Dendritic cells: Bridging innate and adaptive immunity in atopic dermatitis. JACI. 2010 Jan; 125(1): 50-59.
4McKenna K, et. al. Plasmacytoid dendritic cells: linking innate and adaptive immunity. J Virol. 2005 Jan;79(1):17-27.
